Ketamine for depression is showing promise as a treatment, especially when other medications fail. This article explains how ketamine for depression works, its effectiveness, treatment options, and safety.
Key Takeaways
Ketamine, unlike traditional antidepressants, can provide rapid relief from severe depression symptoms, often within hours, making it a promising option for treatment-resistant cases.
Ketamine treatment is offered in various forms, with intravenous (IV) infusion being the most effective, followed by esketamine nasal spray and oral ketamine, each with differing bioavailability and effectiveness.
The cost of ketamine therapy can be a barrier, as most insurance plans do not cover it; therefore, financial assistance programs and policy improvements are necessary to improve access.
Understanding Ketamine and Depression
Depression, particularly severe depression, affects millions worldwide, disrupting lives with its relentless grip. Traditional treatments like SSRIs and SNRIs often require weeks to months to take effect, leaving many sufferers in prolonged anguish. Treatment-resistant depression, where patients experience little to no relief from conventional antidepressant medications or psychotherapy, further complicates the battle against this pervasive psychiatric disorders mental health condition. To effectively treat depression, it is essential to explore alternative therapies and approaches, including a comprehensive treatment for depression.
Ketamine, initially approved for surgical anesthesia in 1970, has emerged as a beacon of hope for those struggling with major depressive disorder and other mental health conditions. Unlike traditional antidepressants, ketamine impacts different neurotransmitter systems, offering an alternative path for those who have not found success with regular antidepressants.
The ketamine molecule works uniquely by influencing neurotransmitters in ways that traditional antidepressants do not. This novel approach has garnered significant attention and research, establishing ketamine therapy as a viable option for treating depression, particularly in cases of treatment-resistant depression.
How Ketamine Works in the Brain
Ketamine works in the brain by triggering a cascade of neurochemical events that lead to its rapid antidepressant effects. One key mechanism involves increasing glutamate levels in the prefrontal cortex, a region crucial for mood regulation. This surge in glutamate enhances synaptic connectivity, effectively rewiring the brain’s communication pathways, which can become impaired in individuals with depression.
Ketamine also blocks specific N-methyl-D-aspartate (NMDA) receptors, which increases excitatory neurotransmission. This blockade stimulates the production of brain-derived neurotrophic factor (BDNF), crucial for synaptic plasticity and overall brain health. Additionally, the activation of the mechanistic target of rapamycin (mTOR) pathway supports protein synthesis, vital for maintaining healthy synaptic connections.
Ketamine’s metabolites, especially hydroxynorketamine, contribute to its antidepressant effects without directly blocking NMDA receptors. This multifaceted approach explains ketamine’s ability to provide rapid relief from depression symptoms, often within hours of administration.
Different Forms of Ketamine Treatment

Ketamine treatment is available in various forms, each with its benefits and limitations. Intravenous (IV) ketamine infusion is the most effective, with 100% bioavailability, meaning the entire dose is absorbed into the bloodstream, providing reliable and immediate relief from depression symptoms. These infusions are monitored by healthcare professionals to ensure patient safety.
Esketamine, a ketamine derivative, is administered as a ketamine nasal spray and must be combined with an oral antidepressant for effectiveness. Although convenient, intranasal ketamine’s bioavailability is lower, ranging from 25% to 50%, making its absorption and effectiveness more unpredictable.
Oral ketamine, while less invasive, has the lowest bioavailability at 16-24%, significantly reducing its effectiveness compared to IV administration. Ketamine treatment generally requires a series of sessions over several weeks to achieve optimal results.
Clinical Evidence Supporting Ketamine Therapy
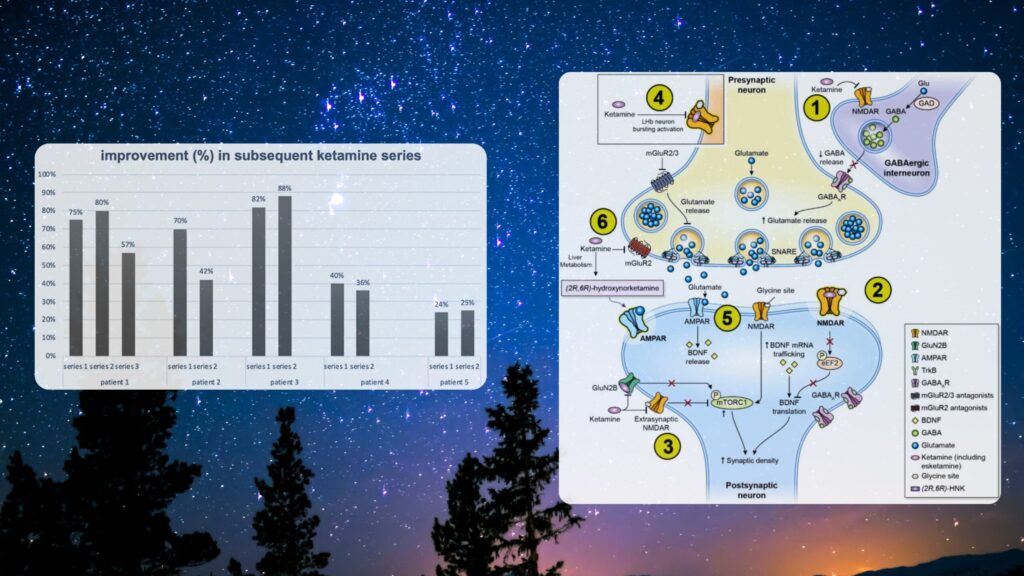
The clinical evidence supporting ketamine therapy is robust and growing. A recent meta-analysis highlighted ketamine’s antidepressant efficacy from the very first day of treatment in both unipolar and bipolar depression. Patients receiving repeated doses over two weeks showed significant and lasting decreases in both anxiety and depression symptoms.
A compelling aspect of ketamine treatment is its rapid onset of action. Unlike traditional antidepressants, which can take weeks to show effects, ketamine can alleviate depressive symptoms within hours. Clinical trials have shown that repeated intravenous ketamine infusions result in sustained improvement in depressive symptoms over 15 days, consistently outperforming placebo groups and providing significant decreases in depression scores.
The long-term safety and effectiveness of ketamine therapy remain areas of ongoing research. Although short-term studies are promising, comprehensive long-term data are needed to fully understand the risks and benefits of this treatment.
Safety and Side Effects of Ketamine

Safety is paramount in ketamine therapy. Common side effects include dissociation, increased blood pressure, nausea, vomiting, and dizziness, highlighting the importance of in-person monitoring to manage any potentially severe reactions.
Dissociation, where patients feel detached from their surroundings or themselves, is a notable side effect that can be distressing for some. Additionally, ketamine can cause sedation and increased high blood pressure, requiring careful monitoring. Patients with a history of substance use disorder may have heightened risks of developing ketamine use disorder due to its euphoric effects.
Despite these risks, ketamine’s safety profile is generally favorable when administered under proper medical supervision. Careful screening and monitoring of patients throughout their treatment journey are essential.
Who Can Benefit from Ketamine Treatment?
Ketamine treatment is not suitable for everyone, but it can be a lifeline for many. Patients with moderate to severe depression, especially those unresponsive to traditional treatments, may be eligible for ketamine therapy. Thorough medical and substance use histories help determine suitability for treatment.
Patients with a history of psychosis or active substance abuse are generally excluded from ketamine treatment due to potential risks. However, those suffering from acute suicidality may be candidates for ketamine infusions due to its rapid action. Patients with bipolar disorder may qualify if their mood is stable.
The decision to pursue ketamine therapy should be made in consultation with healthcare providers, considering all unique risk factors and potential benefits.
The Role of Ketamine Clinics
Ketamine clinic play a pivotal role in delivering this innovative treatment. Typically staffed by a multidisciplinary team of psychiatrists, anesthesiologists, nurses, social workers, and business professionals, these clinics provide comprehensive patient care. However, communication between clinic staff and primary healthcare providers often lacks integration, affecting care coordination.
Inpatient settings for ketamine treatment generally have stricter oversight and protocols compared to outpatient facilities, enhancing treatment safety. Concerns about mail-order ketamine clinics include potential risks associated with compounded ketamine products that may not meet safety standards.
Most independent ketamine clinics have been established since 2019, reflecting an increase in the availability of this treatment option. These clinics are instrumental in making ketamine therapy accessible to those in need.
Comparing Ketamine with Traditional Antidepressants
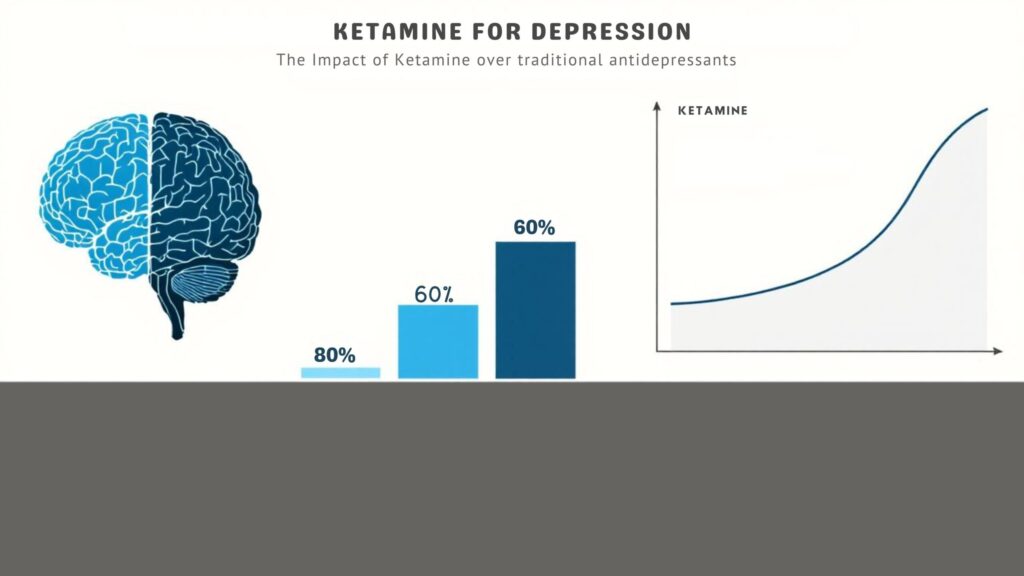
Ketamine contrasts starkly with traditional antidepressants in both mechanism and speed of action. While fluoxetine, the first SSRI approved in the 1980s, often takes weeks to months to show effectiveness, ketamine can alleviate depressive symptoms within hours, providing rapid relief for patients experiencing acute depressive episodes.
For those with treatment-resistant depression, ketamine offers a promising alternative when traditional antidepressants fail. It can also complement traditional antidepressants, potentially improving overall outcomes for patients. Additionally, ketamine typically has shorter and less intense side effects compared to the longer-lasting adverse effects of regular antidepressants.
This rapid and effective approach makes ketamine a valuable tool in the fight against depression, offering new hope for those who have struggled with conventional treatments.
Cost and Insurance Coverage for Ketamine Therapy
The cost of ketamine therapy can be a significant barrier for many patients. Out-of-pocket costs for IV ketamine infusions can generally start around $400 per session, and insurance coverage is often limited. The lack of FDA recognition for generic ketamine as a treatment for mental health conditions further restricts insurance coverage options.
Most private insurance policies exclude ketamine as a mental health treatment, treating it more as an anesthetic. Medicare and Medicaid generally do not cover most forms of ketamine treatment, restricting access for many patients.
Financial assistance options, such as healthcare spending accounts or installment plans, may be available to help with treatment costs. More uniform insurance policies are needed to enhance access to ketamine therapy, ensuring more patients can benefit from this groundbreaking treatment.
Future Directions and Ongoing Research
Research is crucial to understanding the long-term effectiveness and safety of ketamine therapy. Studies focus on how well ketamine maintains remission in patients over extended periods. A longer-term study on nasal ketamine showed positive results, helping participants maintain stable remission after 16 weeks of treatment.
Research is also exploring necessary safeguards to enhance patient safety and minimize risks. A proposed registry combining data from diverse treatment sites aims to capture the long-term effectiveness and safety profiles of ketamine more accurately.
These efforts are essential for ensuring ketamine remains a safe and effective treatment option for mental health conditions in the future, pending fda approval.
Summary
Ketamine therapy is revolutionizing the treatment of depression, offering rapid relief for those who have not found success with traditional antidepressants. Its unique mechanism of action, various forms of administration, and robust clinical evidence make it a promising option for many patients.
As research continues to explore its long-term safety and effectiveness, ketamine is poised to become an integral part of mental health treatment. By addressing both the benefits and challenges of this therapy, we hope to inspire hope and provide valuable insights into the future of depression treatment.
Frequently Asked Questions
How quickly does ketamine work for depression?
Ketamine can relieve depressive symptoms within hours, offering a quick alternative to traditional antidepressants that typically require weeks to take effect.
What are the side effects of ketamine therapy?
Ketamine therapy can cause common side effects such as dissociation, increased blood pressure, nausea, vomiting, and dizziness. It is essential to have in-person monitoring to effectively manage these effects.
Who is eligible for ketamine treatment?
Individuals with moderate to severe depression who haven’t responded to standard treatments are eligible for ketamine treatment, while those with a history of psychosis or active substance abuse are typically excluded.
How much does ketamine therapy cost?
Ketamine therapy typically costs around $400 per session for IV infusions, and insurance coverage is generally limited, though financial assistance options might be available.
Is ketamine therapy safe?
Ketamine therapy, when conducted under appropriate medical supervision, is generally safe. It is crucial to ensure careful screening and monitoring to address any potential side effects and risks.

